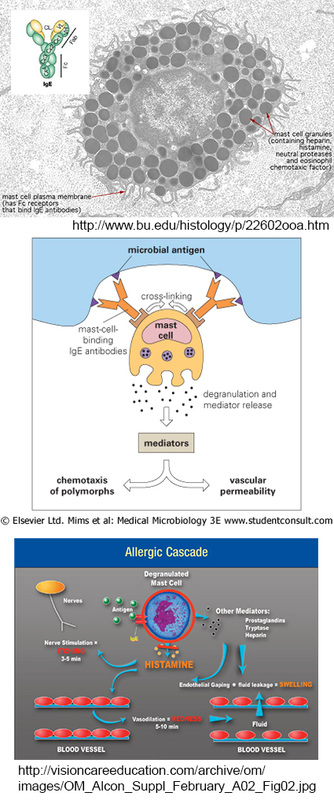
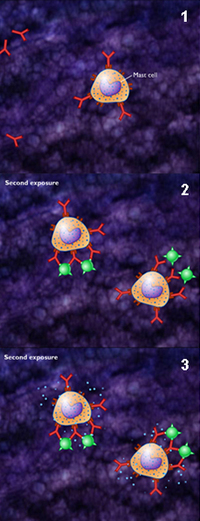
So I'd like to move on to another summer time ailment, at least, for people like me, and that is: mosquito bites! What really interests someone like me who demonstrates a hypersensitivity to the bites, is WHY do the bites swell up so dramatically, and why are they SO itchy that I'd rather scratch myself to the point of bleeding and scarring than leave it alone?
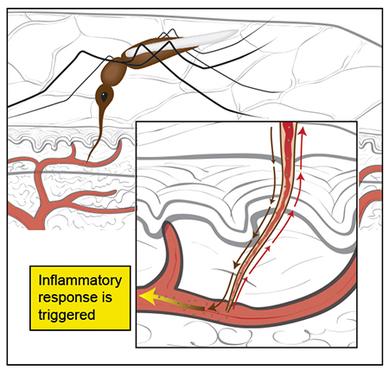
Well, the answer lies in an elegant function of a mosquito's proboscis, its long nose-like instrument that is flexible and thin. It uses this to pierce our skin and then PROBE for a blood vessel, and is so microscopic that we cannot feel it when it goes in. Once it hits the vessel, the object of the game is to suck our blood up through this proboscis, which is also a straw by the way, that the mosquito needs to feed her eggs. But this instrument can simultaneously eject substances into us that prevent blood from clotting; once blood clots, it can't get sucked up through the proboscis.
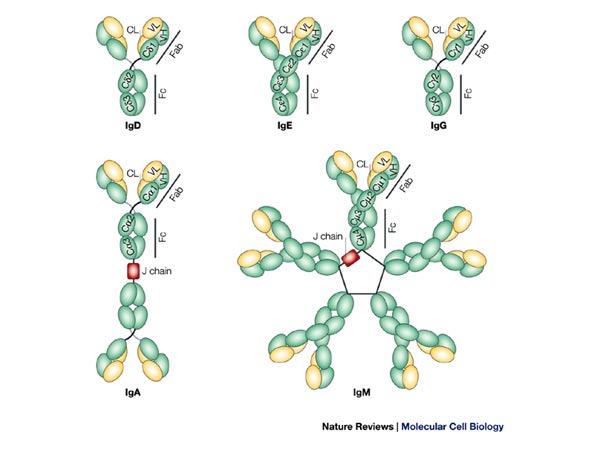
A certain protein also found in their saliva, dubbed rAed a 2, is an allergen, or a substance that causes an allergic reaction. We have not isolated, analyzed, nor identified it sufficiently to create a counter punch to it. So for those of us who are sensitive, right now our only hope is to get bitten more and more in order for our bodies to hopefully become de-sensitized to the allergen. Hmmm, I think I'd rather wear DEET!


 RSS Feed
RSS Feed
